Greetings
We have a month or more of trauma ahead of us and a lot of interesting talks
The idea is to get through the most important and contemporary aspects of trauma management in ED and also to brush on some basic concepts of ATLS that we practice
There is a list of topics to present
this month we will summarise all our talks by leaving comments on this web page
any talks that are stored in open access cloud space (google drive / icloud etc ) will have links on this page
The value of this sort of teaching is that there is documentation of what we are learning and anopportunity for all of us to feedback perspective updates etc . This reflects what WEB 2.0 is all about !!
TOPICs ( to be covered over the month )
THE FAST and EFAST with practical demonstration – Mick (s) Karen et al
MASSIVE TRANSFUSION IN THE EXANGUINATING PATIENT –
PERMISSIVE HYPOTENSION IN TRUAMA – where do we stand – reg /middlegrade talk
CHRASH 2 – medical student
SAFE study (normal saline v chrystaloid ) – CONOR
THE VALUE OF RECTAL EXAM IN TRUAMA – Muhammed
Intercostal drain insertion – Eimhear
Thorocotomy- Karen
www.braintrauma.org guidelines – at least 5 guidelines with interesting topics – pick any even surgical managment – 5 talks
 EXANGUINATING PELVIC TRAUMA – MICK and Safa link to MICKS PELVIC FRACTURE TALK HERE https://www.icloud.com/iw/#keynote/BAKG0mpd7MjKjYCmbMaBN-FZZ-89ia5nmvaF/PELVIC_FRACTURE_negative_fast
EXANGUINATING PELVIC TRAUMA – MICK and Safa link to MICKS PELVIC FRACTURE TALK HERE https://www.icloud.com/iw/#keynote/BAKG0mpd7MjKjYCmbMaBN-FZZ-89ia5nmvaF/PELVIC_FRACTURE_negative_fastTHORACOTOMY – sensible indications- KAREN
THORACTOMY – HOW TO – VIDEO
SHOCK AND SPINAL CORD INJURY ( neurogenic and spinal shock explained )
TRAUMA SCENARIOS – PICK ONE ( OR MAKE A BETTER ONE UP )
– PREGNANT PATIENT POLYTRUAMA
– MASS CASUALTY- > 2 CRITICAL PATIENTS – DISCUSSION ON PLANNING ONCE THE AMBULANCE CALL COMES I
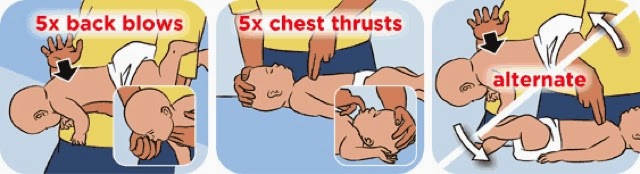
-PAEDIATRIC
POLYTRUAMA – REVIEW OF PALS VALUES /RSI
– GCS 3 BLOWN PUPIL !
-PELVIC FRACTURE