All posts by Michael Sweeney
Opinion piece on Emergency Medicine in Ireland published in The Irish Times
Fergal Hickey’s piece regarding the future of Emergency Medicine in Ireland published in today’s Irish Times
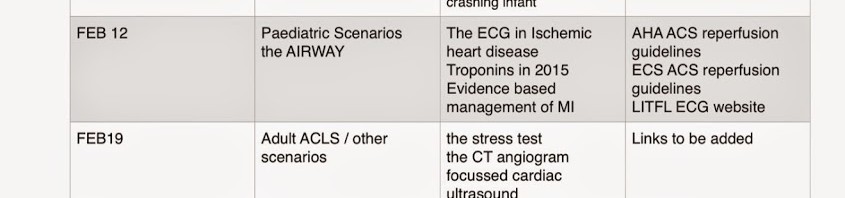
ED teaching for the beginning of the new year
FCEM Success for Karen
Congratulations to Dr Karen Harris, our current SpR, who passed her final FCEM exams today.
All ED staff delighted
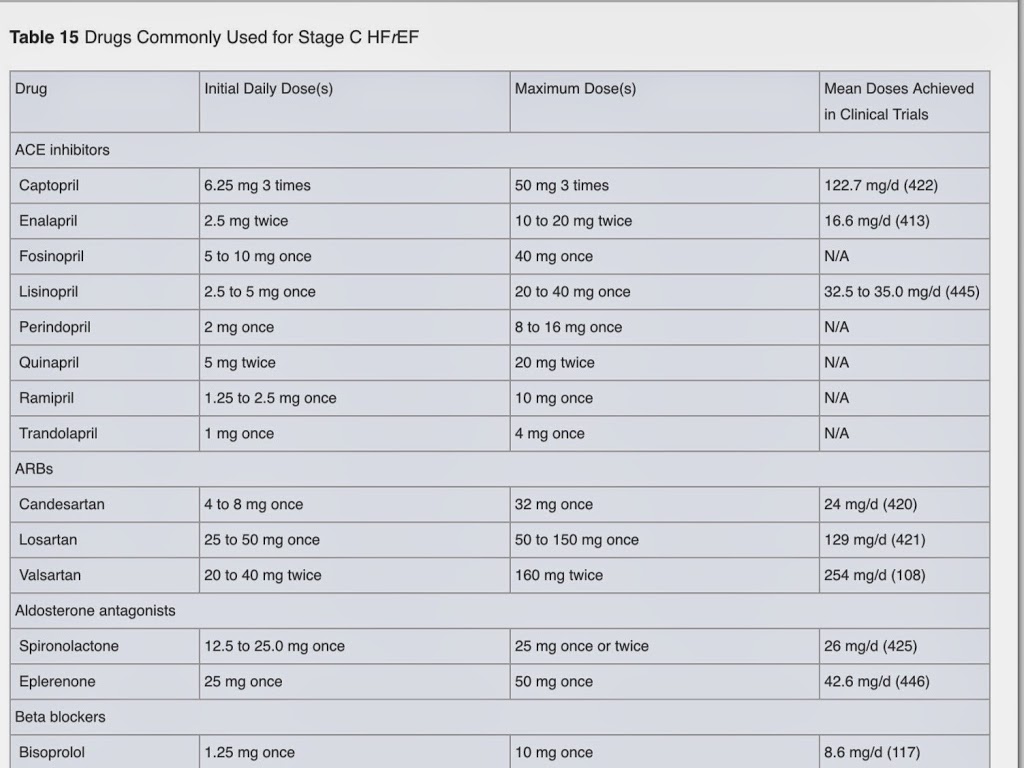
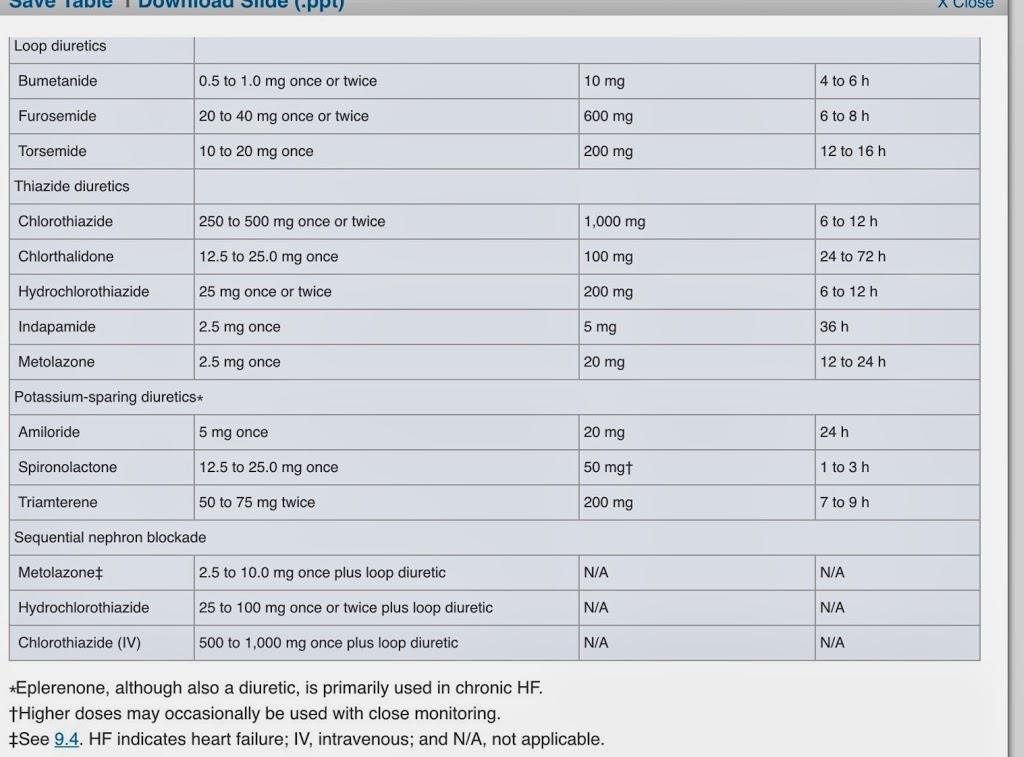
Summary of heart failure talks
. These guidelines are 100s of pages long and reflect the opinion of 100s of clinicians , researchers and patients
Persistent uncontrolled nyhc grades 2-4 :
NOVEMBER DECEMBER TEACHING BLOG FOR SLIGO ED
WELCOME TO SLIGO ED TEACHING BLOG (EMSLIGO.BLOGSPOT.IE) NOV / DEC 2014
The purpose of this blog is to store teaching talks and other information
The idea is that each talk has a 1 page summary. posted here and links to references/websites used
The links on this page are a great start to finding information for your talks
There will be a (very flexible ) five week cycle
Week1 : NCHD / medical student talks – 4 10 minute talks ( strickly 10 mintues as we have short attention span ) .summary posted here(email me your summary with links mickilleen@gmail.com)
Week 2 : NCHD / medical studtent talks
Week 3 : simulaiton training
Week 4: NCHD / medstudent talks
Week 5: M/M ( review of interesting patients in Resus – keep a patient sticker so you can look up what happened to your patient and present it ) A middlegrade doc or consultant will oversee this .
There will be an OSCE type quiz on topics from these talks ( we will ask each presenter to create an OSCE type question ) this will happen once a term ( so pay attention to the blogsite !)
TOPICS WILL INCLUDE : (red denotes what we have partially covered so far )
1) Management of Acute cardiac emergencies including ACLS review
2) Management of acute respiratory emergencies including Airway management and RSI )
3) Management of acute Neurological Emergencies including CVA (SAH/thrombolysis debate / stroke and TIA guidelines / syncope )
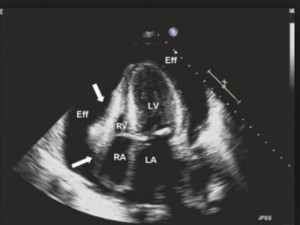
4) Vascular Catastrophes . AAA/ dissection / cardiac Tamponade
5) Trauma management – Recent updates eg ICEM , Damage control resuscitation / crash 2 trial / TTM trial
6) Orthopaedic injuries ( pelvis / longbone / hand and foot / soft tissue injuries to shoulder , knee , wrist and ankle
7) The focussed clinical exam in 2014 – Different Joints / formal Cardiac exam / neurological examination .
8) ULTRASOUND TRAINING – (THREE LECTURES , LOGGING SCANS , SUPERVISION AND TESTING )
9) Paediatric Emergencies ( Assessment of the unwell child / PALS / APLS / APLS review / NAI
10)Interpretation and management of Acute Electrolyte disturbances (hyperkaleamia / acid base / hyponatremia / Hypernatremia / DKA / Honk / Acute renal failure )
11) The critically ill patient – Sepsis bundles / BOIC / Post cardiac arrest management / post intubation check list / inotropes / antibiotics in serious sepsis
12) Toxicology – general approach / Specific and common life-threatening overdoses. Seratonin and anticoholinergic syndrome
THIS MONTHS TOPICS
WEEK ONE ( 13th Nov) – SUMMARY OF ESSENTIALS OF EM CONFERANCE (no NCHD TALKS)
WEEK TWO ( 20 November ) 4 talks in total :
—————————————————————————————————————–
Week THREE
Simulation training
week 5
M/and M
Sligo Emergency Department shortlisted for two 2014 Healthcare Innovation Awards
Sligo ED has been shortlisted in two categories for the 2014 Healthcare Innovation Awards.
Innovation – Clinical Area : A safe protocol for paediatric procedural sedation in the ED
Patient Experience: ART in the waiting room
Congrats to all staff involved
http://www.healthawards.ie/2014-shortlist/
OCTOBER TEACHING – week 1 Sodium
Moving on to medical emergencies , this weeks teaching is brought to you by the elelement Na !
Last week of september -Trauma round up
This week we have the following / talks discussions
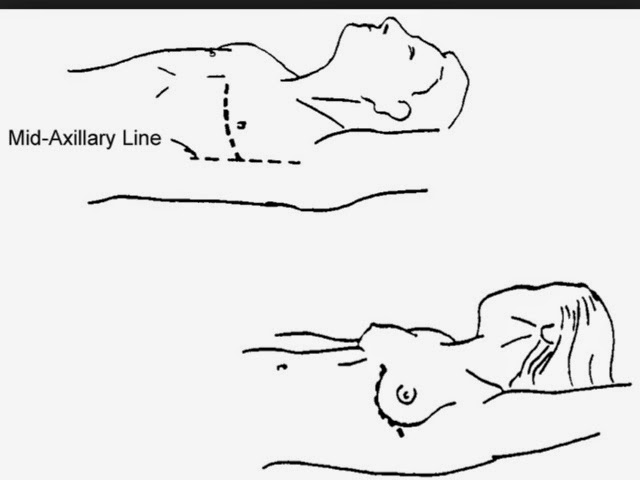
4) Ultrasound guided nerve blocks in the ankle and the femoral nerve block
LINK TO powerpoint on Nerve blocks to lower limb
( useful really only for references and diagrams of relevent nerves )
click on image below to be forwarded to icloud version of PPT
summary to this weeks talks
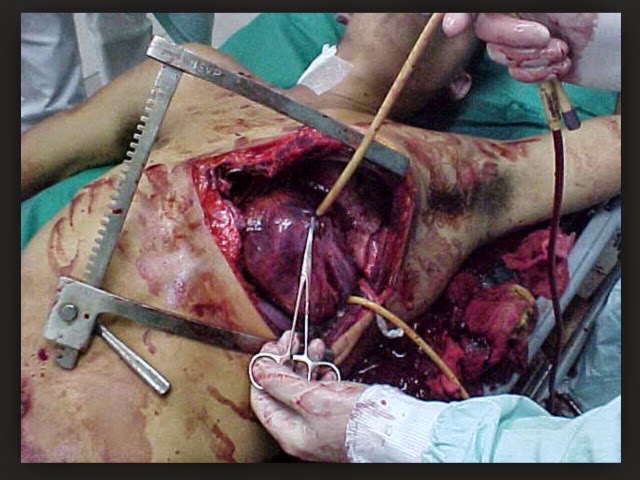
ED THORACOTOMY